May 21, 2020
by Ceci Connolly
 The ongoing COVID-19 public health crisis is causing an unprecedented shift in the way Americans view and access health care. A nation of anxious but adaptable consumers carries major implications for a health sector that represents 18 percent of GDP.
The ongoing COVID-19 public health crisis is causing an unprecedented shift in the way Americans view and access health care. A nation of anxious but adaptable consumers carries major implications for a health sector that represents 18 percent of GDP.
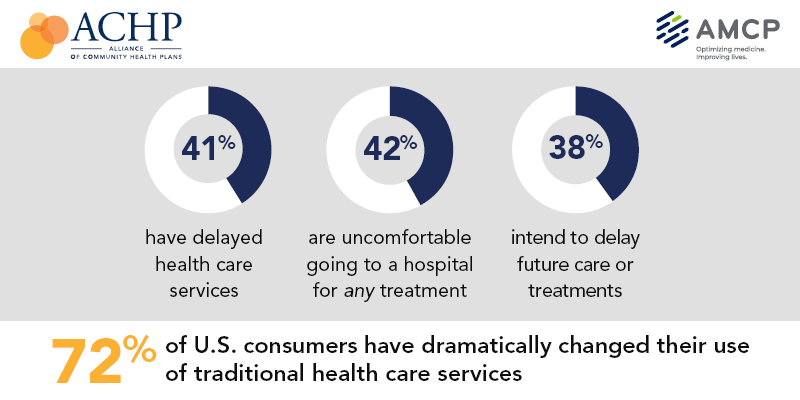
Citing concerns about coronavirus, 72 percent of U.S. consumers have dramatically changed their use of traditional health care services during the pandemic, with many delaying in-person care and embracing virtual options, according to a new national survey released by the Alliance of Community Health Plans (ACHP) and AMCP, conducted by Leede Research.
Respondents cite their doctor as the most trusted source of information about the novel coronavirus, but only 31 percent feel “comfortable” visiting their doctor’s office, leading to significant changes in how, when and where they plan to interact with the health profession.
In fact, 41 percent have delayed health care services and 38 percent intend to delay future care, treatment and procedures.
However, these concerns, coupled with continued trust in providers, has resulted in a potential bright spot. For example, 28 percent report having used some type of virtual care in the past three months, nearly tripling previously documented averages. And an overwhelming 89 percent of those who have used telehealth, including phone and Internet, were satisfied or very satisfied with the experience.
ACHP’s nonprofit plans, in tandem with their provider partners, are quickly pivoting to provide new or additional telehealth options in light of COVID-19. The majority of plans have deployed or expanded these services and are waiving related out-of-pocket copays to help address immediate member needs.
It’s also worth noting that as unemployment rises, so does anxiety about losing health insurance. Nearly a quarter of respondents with insurance are worried about losing coverage within the next six months. Among uninsured respondents, 38 percent expressed a willingness to pay $75-$300 per month for coverage.
This is why ACHP developed a comprehensive proposal that would assemble all the pieces needed to fill the entire coverage puzzle, including a federal Special Enrollment Period, a Medicaid Stabilization Fund, Premium Grace Period protections, reinsurance and risk corridors and the expansion of the Health Coverage Tax Credit.
Additionally, the majority of survey respondents believe it is likely or very likely there will be a resurgence of coronavirus in the coming months, creating uncertainty about their future care plans, in turn causing fresh worries for care providers.
As consumer anxieties rise, we see an industry grappling with how best to address coverage and care. These insights provide a clear illustration of consumers’ attitudes toward the current health care environment and the work and potential opportunities that lie ahead for an industry already stretched to meet the demands of the moment.
Information on efforts of ACHP plans and their affiliated systems during this public health crisis is available here.
Please contact Dan Lemle with any questions.
Consumer Behavior Resources
ACHP & AMCP Joint Press Release


































