October 29, 2020
by Dr. Connie Hwang and Ginny Whitman
Telehealth has become a lifeline for patients, providers and health plans. The abundance of positive experiences makes it impractical to imagine why we would ever go back. Virtual care highlights the value of seamless, integrated care delivery. Optimizing the virtual platform potentials, from phone calls to remote patient monitoring technology, providers have improved preventive medicine, triaged urgent care needs and managed complex chronic conditions, all in the face of a pandemic. Our collective telehealth experience demonstrates that we must determine how to continue these valuable, cost-effective services beyond the current crisis.
Concrete steps to solidify a financially sustainable path forward are key. ACHP has developed two approaches to telehealth reimbursement to improve access and ensure telehealth payment is aligned with high-quality care. These potential payment models offer a starting point for the industry to explore full, value-based telemedicine in Medicare, which serves a population dependent on virtual care. We envision these approaches as a starting point for stakeholders to ensure telehealth remains an available and affordable option for all.
Current barriers
A number of barriers in the Medicare program currently prevent virtual care from reaching its full potential. Overcoming outdated and insufficient infrastructure, concern about over-utilization and the fee-for-service system built on volume is critical to advancing robust telehealth adoption. ACHP’s proposed models offer a thoughtful transition to value-based arrangements necessary for a sustainable telehealth program.
 Next Steps to Sustainability
Next Steps to Sustainability
Any approach to a financially sustainable telehealth program in Medicare must consider three things:
- The time it will take to transition to a new payment model,
- How to balance in-person and virtual care, and
- How to safeguard the high-quality nature of telehealth services.
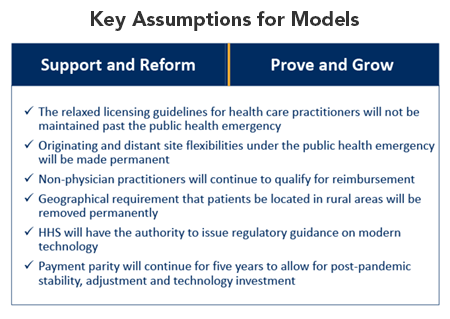
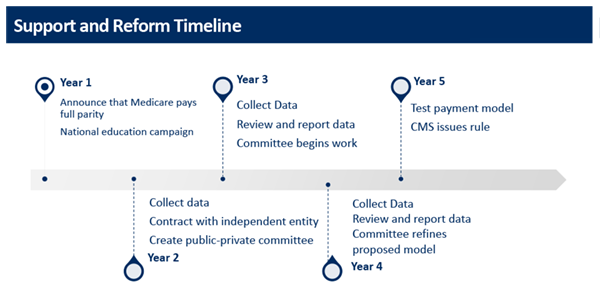
Both of ACHP’s potential payment models include a three to five-year, phased-in approach to implementing a permanent payment structure. This assumes that, although not sustainable in the long-run, continuing payment parity for telehealth in the near term is needed for post-pandemic stability, adjustment and technology investment. Providers also need time to collect data as non-emergency health care delivery normalizes, helping plans, providers and patients evaluate the services that work best via virtual care.
Model One: Support and Reform
ACHP’s Support and Reform approach proposes Medicare offer full payment parity for telehealth for five years post-public health emergency. Over the five years, significant utilization data would be collected in order to determine the appropriate balance of in-person versus virtual care, based on cost-effectiveness and health outcomes.
This data collection effort will contribute to a “matrix of care” for each medical specialty, ensuring Medicare is only reimbursing for the highest quality services. Providers will be paid a fixed amount for each patient they see – on a per member per month basis –rewarding higher-quality services most effective in a virtual setting with additional payments.
This “matrix of care” would also utilize existing quality measurement tools, such as HEDIS, to evaluate types of care most appropriate for telehealth. Under this model, if a high proportion of telehealth visits result in excessive follow-up in-person care, the service will be demoted and therefore receive a lower payment.
Model Two: Prove and Grow
The Prove and Grow approach would allow for incremental growth of telehealth through the reinvestment of capital and support to specific areas of lower-capitalized types of care, including primary care. Prove and Grow proposes Medicare pay full parity for telehealth services for five years beyond the public health emergency, but for a limited number of services, including chronic care management, behavioral health and preventive care.
After the five years, all provider reimbursement in this model would reduce to 80 percent of in person visits. To maintain that level of reimbursement providers would have to report on prevention and wellness strategies demonstrating high performance in quality and cost management. This measurement of cost savings has the potential to result in bonus payments that may be reinvested into telehealth advancements, primary care and/or geriatric care.
Time for Action
It is time for a permanent telehealth benefit in Medicare. To make this a reality, it is critical that we take concrete steps forward on an evidence-based payment structure that focuses on value, access and affordability. ACHP seeks input and insight from industry partners, consumer advocates and all interested thinkers to hone these models. It is essential that industry partners and stakeholders share in this commitment as we navigate new demands of the health care system throughout and beyond the pandemic.
For those who are interested, ACHP will convene a stakeholder discussion this December in order to move these ideas forward.
For more information, please see ACHP’s White Paper: Potential Models for Medicare Telehealth Payment Post COVID-19. Contact Ginny Whitman at vwhitman@achp.org to participate in a stakeholder roundtable or to discuss the white paper.
Learn How ACHP is Championing Telehealth
Learn More about ACHP’s Efforts to Enhance Medicare Advantage